By Jerrod Ullah, CEO & Founder
The expiration of continuous enrollment under the Families First Coronavirus Response Act has triggered a significant transition. This dynamic shift has brought forth challenges for both patients and healthcare organizations. The consequences of inaction are far-reaching, encompassing erratic member coverage, costly churn, uncovered care, unattended visits, and billing delays.
The initiation of the “unwinding” process by the federal government serves to redetermine the eligibility of all Medicaid recipients. This follows the automatic enrollment of individuals, eligible or not, under COVID provisions in the Families First Coronavirus Response Act.
The Department of Health and Human Services (HHS) estimates that up to 15 million people will be disenrolled, with 6.8 million potentially still eligible. This ongoing process, set to conclude in May, poses a considerable challenge, as seen in Georgia, where approximately 2.8 million people on Medicaid await eligibility reassessment. Despite significant efforts to minimize coverage termination, more work remains to be done.
Recent updates provided by Georgia Department of Human Services Commissioner Candice Broce showed that there have been 550,444 Medicaid terminations and 543,967 renewals in their state. However, no breakdown of determinations was provided, leaving questions about the reasons, and possibility of clerical errors, related to some of them.
Another factor that can’t be discounted is that certain demographic groups face more barriers and heightened risks during this unwinding period — including those who have moved, immigrants, individuals with limited English proficiency, people with disabilities, and older adults. As states resume redeterminations and disenrollments, these individuals may experience gaps in coverage due to barriers in completing the renewal process, even if they remain eligible.
Despite the progress made in increasing Medicaid coverage, the resumption of disenrollments is expected to reverse these gains, potentially increasing the number of uninsured individuals.
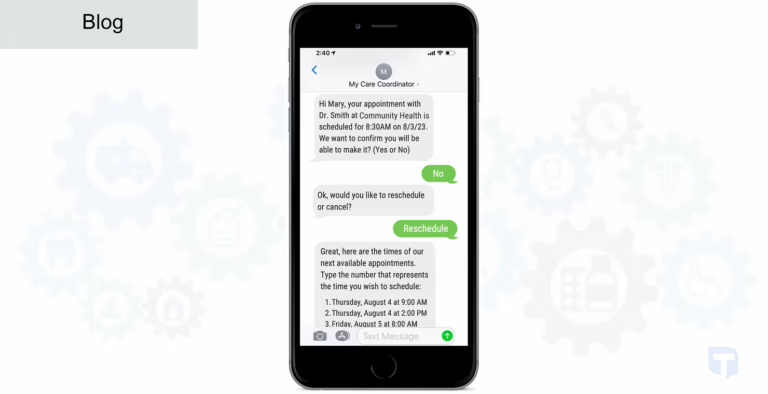
At HealthTalk A.I., we have the privilege of partnering with many Community Health Centers (CHCs). These organizations play a vital role in guiding patients through the Medicaid re-enrollment process and providing education on alternative Marketplace coverage options. To navigate this challenging period, maximizing streamlined renewal processes is crucial — and our AI Patient Engagement solution helps do just that.
- Proactive Medicaid Management: Reinstate coverage for lapsed members, preventing uninsured visits.
- Automated Oversight: Actively manage coverage for Medicaid, commercial, and self-pay populations.
- Informed Decision-Making: Provide comprehensive insights into coverage across your entire population.
- All Language Support: Promotes health equity by allowing patients to communicate in their preferred language.
As we navigate the expiration of continuous enrollment for Medicaid recipients, let’s seize this opportunity to enhance patient experiences and drive positive outcomes. Don’t let it be a hurdle; let it be a catalyst for progress.